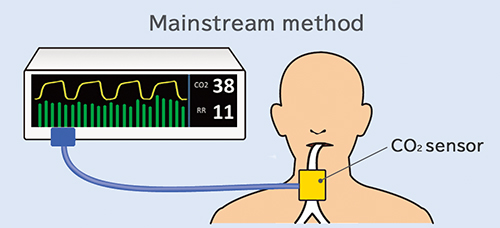
At Nihon Kohden, we have always used the mainstream method to measure CO_{2}.
The reason is that in general, the mainstream method has superior responsiveness and stability and can better respond to rapid and low-volume breathing. Because of the long-term stability of the measurements and the sensors' fast response time, mainstream CO_{2} sensors are widely used in both ICUs, where patients are connected to ventilators for long periods of time, and in emergency resuscitation, where speed is of the essence.
However, because large sensor components are directly attached to the mouth, mainstream CO_{2} sensors could not be used for patients receiving supplementary oxygen through an oxygen mask, or for intubated* patients. Also, because the tubes used for intubation of neonates are very thin, it was difficult to attach a sensor because it caused the tube to bend. Extracting blood and measuring the CO_{2} in the blood was possible but frequent extraction of blood is a large burden on a small body.
*Tracheal intubation: Insertion of a tube into the trachea through the mouth for mechanical ventilation during surgery under general anesthetic or in an ICU.
To solve these kinds of problems, we started developing a small, lightweight sensor that could be used by both intubated and non-intubated patients, and even by neonates with thin breathing tubes. After trying many different shapes, we succeeded in creating a small, lightweight design that only weighed 4g. With this CO_{2} sensor, we were able to measure the end-tidal CO_{2} of a non-intubated neonate using the mainstream method while the neonate was receiving supplementary oxygen (such a through a mask).
Further, the small size and light weight of this sensor makes it possible to measure the CO_{2} of a patient wearing a mask. For that reason, we started work on developing a new type of oxygen mask and succeeded in creating a revolutionary new product, which is a mask that can measure CO_{2} at the same time as supplying oxygen.
This small CO_{2} sensor can be used to monitor the patient condition in a wide range of situations.